Successful steps taken on path to HIV cure
 A new technique is being developed which can destroy HIV infection while leaving other cells untouched.
A new technique is being developed which can destroy HIV infection while leaving other cells untouched.
A recent experiment has seen HIV-infected cells completely wiped out in blood samples taken from patients already treated with antiretroviral therapy.
Highly active antiretroviral therapy (HAART) has allowed patients infected with HIV to live normal lives, by suppressing the replication of the virus in the body. But despite the success of HAART in reducing the burden of the disease, there is a belief that pools of latent infected cells can persist in the body, preventing the possibility of a permanent cure.
“In an HIV patient on HAART, drugs suppress viral replication, which means they keep the number of viral particles in a patient's bloodstream very low. However, HAART cannot kill the HIV-infected cells,” said Dr Ekaterina Dadachova, the lead author of a new study and professor of radiology, microbiology and immunology at Albert Einstein College of Medicine in the Bronx, New York.
“Any strategy for curing HIV infection must include a method to eliminate viral-infected cells.”
That is what the new approach has done, by using radioimmunotherapy (RIT) administered to blood samples from 15 HIV patients treated with HAART at an AIDS research centre.
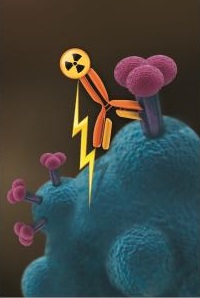
RIT uses an antibody designed to recognise and bind to a specific cell antigen paired with a radioactive isotope.
When injected into the patient's bloodstream, the laboratory-developed antibody travels to the target cell where the radiation is then delivered.
“In RIT, the antibodies bind to the infected cells and kill them by radiation,” Dr. Dadachova said.
“When HAART and RIT are used together, they kill the virus and the infected cells, respectively.”
For the recent study, the team paired a normal RIT antibody (mAb2556) which targets a protein expressed on the surface of HIV-infected cells, with the radionuclide Bismuth-213.
Researchers found the RIT killed HIV-infected lymphocytes previously treated with HAART, reducing infection in the samples to undetectable levels.
“The elimination of HIV-infected cells with RIT was profound and specific,” Dr. Dadachova said.
“The radionuclide we used delivered radiation only to HIV-infected cells without damaging nearby cells.”
Further testing showed experimentally that the same treatment is capable of crossing the blood-brain barrier and killing HIV-infected cells, without any overt damage to the barrier or brain itself.
“Antiretroviral treatment only partially penetrates the blood brain barrier, which means that even if a patient is free of HIV systemically, the virus is still able to rage on in the brain, causing cognitive disorders and mental decline,” Dr. Dadachova said.
“Our study showed that RIT is able to kill HIV-infected cells both systemically and within the central nervous system.”
Excitingly, clinical trials are the next step for Dr Dadachova’s team.








 Print
Print