Stick to the script to fight bacteria back
 Research is pretty fast - but bacterial evolution is faster, a University of Adelaide drug expert says.
Research is pretty fast - but bacterial evolution is faster, a University of Adelaide drug expert says.
Dr Ian Musgrave from the University's School of Medical Sciences says whenever a new antibiotic is developed, harmful bacteria hastily evolve resistance within a very short period of time.
He says some pharmaceutical groups are abandoning antibiotic research and development because they simply cannot keep up.
“There's no doubt that evolution is winning the antibiotics arms race.
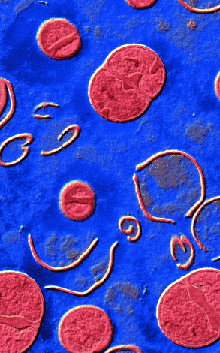
“Bacteria are very good at mutating and developing resistance. What's more, bacteria can easily swap DNA, so these resistance mutations can be effectively 'downloaded' from one bacteria to the next. Bacteria can acquire multiple resistance genes this way,” says Dr Musgrave, a Senior Lecturer in Pharmacology.
“We can attack the metabolic pathways bacteria use, we can attack their DNA replication, or we can bust open their cell walls, but each time scientists develop something new, bacteria will evolve so that the same drugs might not be as effective in the following years. It's a vicious cycle, and we can't continue on it.”
As Jeff Goldblum said in the 1993 documentary Jurassic Park; “I'm simply saying that life, uh... finds a way.”
Dr Musgrave says many drug companies are giving up on antibiotics. He believes antibiotic research and drug development is in a slump, seemingly becoming less profitable and leading to a lack of effective new drugs on the market.
There are a few things drug companies and patients could do to take some ground back in the on-going battle with biology.
Multi-drug cocktails such as those employed for HIV patients could help, as the several-pronged approach confronts bacteria in different ways simultaneously.
“However, this kind of treatment is likely to be expensive for the patient and could lead to additional adverse drug events,” Dr Musgrave says.
For the individual, actually completing an entire course of antibiotics would help slow bacteria’s rise to resistance, in line with the messages of Antibiotic Awareness Week.
“Many people start taking antibiotics but then they feel better and don't see the point in taking them anymore. The point is, they need to kill off all the harmful bacteria. If they don't do this, the bacteria can rapidly build up again and become resistant to the drug,” Dr Musgrave said.
The final piece of advice from key authority on the topic is for GPs to make sure they are not prescribing antibiotics for uncomplicated viral conditions.
“Anything we can do to limit the amount of unnecessary antibiotics in the community will be helpful in preventing resistance,” he said.
“For example, the use of antibiotics in agriculture is a controversial issue, and this can lead to resistant strains of disease that pass from animals to humans.”
Dr Musgrave is one of a range of speakers presenting at Antibiotic Awareness Week events, which started on Monday.








 Print
Print