Programmed place in new age of antibiotics
 A team in the US has reported some success in the quest to create the next generation of specifically-targeted, individually-customised antibiotics.
A team in the US has reported some success in the quest to create the next generation of specifically-targeted, individually-customised antibiotics.
It is a strange time for antibiotics in healthcare, as they are still the go-to treatment in many cases, despite studies routinely showing that resistance is growing while new formulas are not emerging fast enough to cope.
But now, researchers at Rockefeller University are working on a smarter antibiotic - a ‘programmable’ drug that selectively targets the bad bacteria, particularly those harbouring antibiotic resistance genes, while leaving other, more innocent microbes alone.
“In experiments, we succeeded in instructing a bacterial enzyme, known as Cas9, to target a particular DNA sequence and cut it up,” says lead researcher Luciano Marraffini, head of Rockefeller’s Laboratory of Bacteriology.
“This selective approach leaves the healthy microbial community intact, and our experiments suggest that by doing so you can keep resistance in check and so prevent certain types of secondary infections, eliminating two serious hazards associated with treatment by classical antibiotics.”
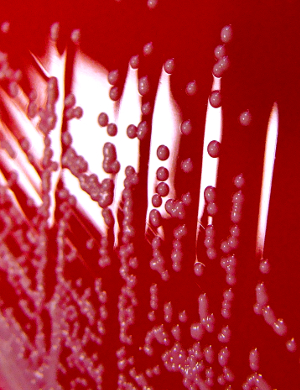
In initial experiments, the team targeted a strain of the common skin and respiratory bacteria Staphylococcus aureus, which was resistant to the antibiotic kanamycin.
The programmed enzymes targeted a part of the resistance gene to kill most of the resistant Staph, but left the kanamycin-susceptible Staph behind.
Bacteria share genes, including those for drug resistance, in the form of rings of DNA known as plasmids. In a second series of experiments, researchers turned the technique on tetracycline resistance-harbouring plasmids in a strain of the potentially deadly multidrug resistant bacteria Staphylococcus aureus (MRSA).
Not only did the resistant cells become sensitive to tetracycline after Cas9 destroyed the plasmids, but the arrival of Cas9 in other Staph cells acted as an immunisation, preventing them from taking on resistance-carrying plasmids.
In a final set of experiments, the team confirmed their test tube results on living skin, by using the tehcniques to selectively kill kanamycin-resistant Staph infecting the shaved backs of mice.
The results are extremely promising, but the delivery system needs improvement.
The researchers used bacteria-infecting viruses to inject the programmed Cas9 enzymes into the bacterial cells, but these viruses only attack specific types of cells. They now need to devise a less discriminating method of delivery before the technology can be used to develop a new class of antibiotics.








 Print
Print