New depth for genetic checks sees Parkinson's in a petri
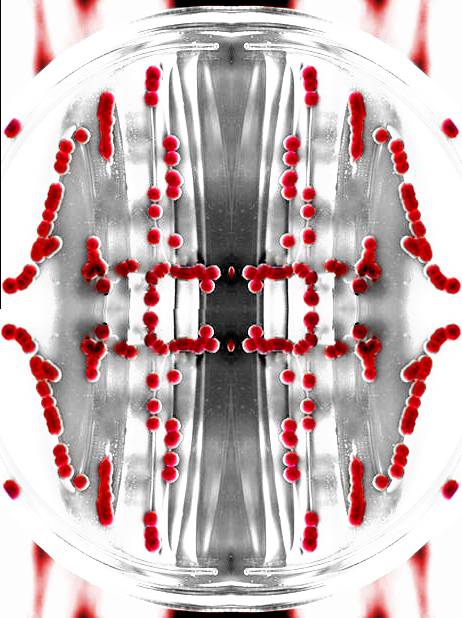 A research team led by The New York Stem Cell Foundation (NYSCF) Research Institute has created a human stem-cell disease model of Parkinson’s disease in a dish.
A research team led by The New York Stem Cell Foundation (NYSCF) Research Institute has created a human stem-cell disease model of Parkinson’s disease in a dish.
The big breakthrough has many implications for Parkinson’s research, as it allows new treatment methods to be tested in a safe environment.
The petri dish analogue was made possible through detailed study of specific patients: a pair of identical (monozygotic) twins, one affected and one unaffected with Parkinson’s disease; another unrelated Parkinson’s patient; and four healthy control subjects.
Researchers were able to observe key features of the disease in the laboratory, specifically differences in the patients’ neurons’ ability to produce dopamine, the molecule that is deficient in Parkinson’s disease.
Already, the scientists have identified a potential strategy for developing novel therapies for Parkinson’s disease.
Most believe Parkinson’s comes from a combination of genetic and non-genetic factors, and it has no completely effective therapy or cure.
DNA mutations resulting in the production of a specific enzyme called glucocerebrosidase (GBA) have been linked to a five-fold greater risk of developing Parkinson’s disease; however, only 30 per cent of individuals with this mutation have been shown to develop Parkinson’s disease by the age of 80.
The discord suggests that multiple factors contribute to the development of Parkinson’s, both genetic and non-genetic factors.
In the latest study, published in Cell Reports, a set of identical twins, both with a GBA mutation, provided a unique opportunity to evaluate and dissect the genetic and non-genetic contributions to the development of Parkinson’s in one twin, and the lack of the disease in the other.
The scientists made induced pluripotent stem (iPS) cells from skin samples from both twins to generate a cellular model of Parkinson’s in a dish, recapitulating key features of the disease, specifically the accumulation of α-synuclein and dopamine deficiency.
After detailed analyses, researchers found that the dopamine-producing neurons from both twins had reduced GBA enzymatic activity, elevated α-synuclein protein levels, and a reduced capacity to synthesise and release dopamine.
In comparison to his unaffected brother, the neurons generated from the affected twin produced less dopamine, had higher levels of an enzyme called monoamine oxidase B (MAO-B), and poor ability to connect with each other.
The investigation suggested that a combination therapy for the affected twin may be possible by simultaneously targeting these two enzymes.
“The subject of Parkinson's disease discordant twins gave us an incredible opportunity to utilise stem cell models of disease in a dish to unlock some of the biological mechanisms of disease,” said Dr. Scott Noggle, NYSCF Vice President, Stem Cell Research.
Working with these various different groups and scientists added to the depth and value of the research and we hope our findings will be applicable to other Parkinson's disease patients and other neurodegenerative disorders.”
More information is available from the NYSCF.








 Print
Print