Custom cancer treatments tested
 The idea of using a cancer patient's own immune cells to create a personalised vaccine is becoming reality.
The idea of using a cancer patient's own immune cells to create a personalised vaccine is becoming reality.
Promising results have emerged from two early-stage human trials in the USA and Germany, which showed that these cancer vaccines appear to be a safe approach for treating skin cancer.
Developing effective cancer treatments that destroy tumour cells without damaging healthy cells has long been a challenge.
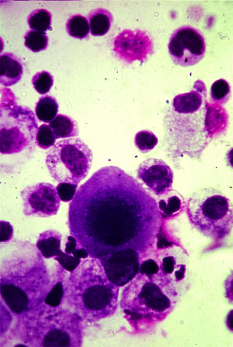
Cancer immunotherapy approaches, which mobilise a patient’s immune system to specifically target cancer cells, have shown promise, but each patient’s tumour has a unique set of mutations that must first be identified, so individually tailored vaccines are needed.
Research leader Catherine Wu and colleagues have reported on a Phase 1 clinical trial of a cancer vaccine that targets up to 20 personalised tumour neo-antigens (targets for an anti-tumour immune response).
They found that the vaccine was safe and induced antigen-specific immune responses in the participants.
Four of the six patients treated with the vaccine showed no recurrence at 25 months, while the other two participants, with progressive forms of melanoma, were later treated with another type of so-called ‘checkpoint therapy’ (anti-PD-1 therapy) and underwent complete tumour regression.
In a separate paper, Ugur Sahin and co-authors report the first-in-human application of a personalised RNA-based vaccine approach, which targets cancer antigens called neo-epitopes, in 13 patients with melanoma.
In all patients, the authors show that the vaccine boosts immunity against some of the patients’ specific tumour antigens, and in two patients, infiltration of vaccine-induced T cells into tumours was observed.
Eight of the 13 patients remained tumour-free at 23 months. Five patients had tumour relapses before starting neo-epitope vaccination. Two of these patients experienced objective responses after neo-epitope vaccination and one patient experienced a complete tumour regression response after sequential administration of neoepitope vaccination and of anti-PD-1 therapy.
“Controlled, randomised Phase 2 clinical trials with more participants are now needed to establish the efficacy of these vaccines in patients with any type of cancer that has enough mutations to provide sufficient neoantigen targets to enable this type of approach” writes researcher Cornelius Melief.








 Print
Print