AIHW measures COVID effects
 The Australian Institute of Health and Welfare (AIHW) has released a new report into the broad health effects of COVID-19 on Australians so far.
The Australian Institute of Health and Welfare (AIHW) has released a new report into the broad health effects of COVID-19 on Australians so far.
The study covers 2020 and early 2021, and includes analyses of the years of healthy life lost, international comparisons and impacts on population groups, mental health and the health system.
The report includes data from a range of sources covering 2020 and some which cover up to June 2021. It does not include data from the latest wave of cases that began in June 2021, dominated by infections of the Delta variant.
“As the COVID-19 situation continues to evolve rapidly and we face challenges such as the emergence of new variants of the virus, it is important we look holistically at the direct and indirect health effects of the pandemic on Australians,” says AIHW spokesperson Dr. Lynelle Moon.
During the first year of the pandemic, Australia avoided the level of health impacts seen in many other countries, where there were large numbers of severe cases and deaths.
If Australia had experienced the same crude case and death rates as Canada, Sweden or the United Kingdom, by early April 2021 there would have been between 680,000 and 2 million cases instead of the 29,000 that did occur, and between 16,000 and 48,000 deaths.
Conversely, if Australia had the same crude case and death rates as New Zealand, there would have been around 18,000 fewer cases and 780 fewer deaths.
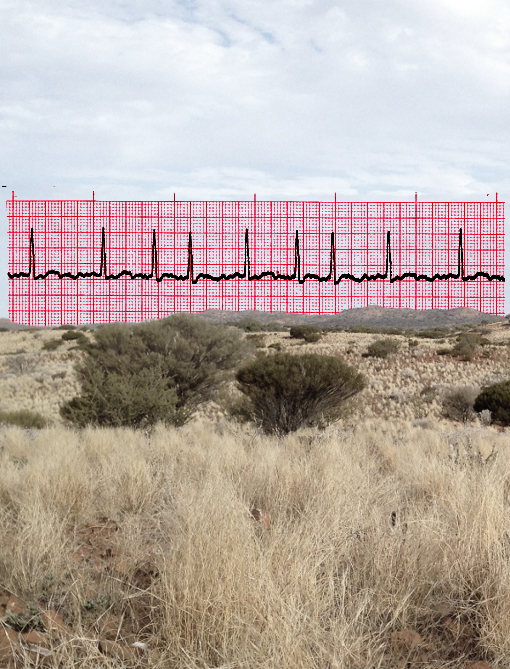
The report uses burden of disease analysis to look at the number of healthy years of life Australians who contracted COVID-19 may have lost.
“There were just over 8,400 disability-adjusted life years (DALYs) lost in 2020 from COVID-19 in Australia and 97 per cent of this disease burden was from fatal cases,” Dr Moon says.
“This is much lower than the burden due to leading diseases in Australia.
By comparison, coronary heart disease (CHD) was responsible for around 312,000 DALYs and respiratory infections for 80,500 DALYs in 2018.
“COVID-19 would rank about 135th out of 219 diseases in terms of total burden of disease.”
During 2020, 7 per cent of all COVID-19 cases in Australia and 75 per cent of all deaths were in people living in residential aged care facilities.
Up to early July 2020, it is estimated that health care workers in Australia were 2.7 times as likely to contract COVID-19 as the general community.
“People living in the lowest socioeconomic areas had COVID-19 mortality rates 2.6 times higher than for people living in the highest socioeconomic areas,” Dr Moon said.
“The reason for these inequalities are complex, and interpreting this finding is complicated by the majority of deaths being in residential aged care facilities. However, these socioeconomic differences do not appear to be driven by aged care facilities being over-represented in lower socioeconomic areas.”
The COVID-19 pandemic in Australia also appears to have increased levels of psychological distress, particularly for adults aged 18 to 45.
“By April 2021, the average level of psychological distress had returned to pre-pandemic levels, however continued to be higher for young people,” Dr Moon said.
Between April and June 2020 (during which time lockdowns and other restrictions were in force in many parts of the country), Australian Bureau of Statistics Survey data shows some Australians increased their physical activity, including exercise. However, a similar number of people decreased their physical activity.
The full report is accessible here.








 Print
Print