Drug switch could cut golden staph
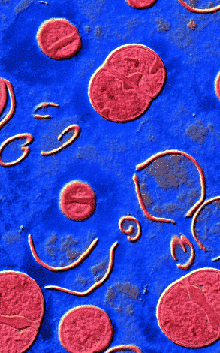 Experts say hospitals should reduce broad-spectrum antibiotic use in the fight against golden staph.
Experts say hospitals should reduce broad-spectrum antibiotic use in the fight against golden staph.
In 2017, an international shortage of piperacillin/tazobactam (PT) – an antibiotic used to treat pelvic inflammatory disease, intra-abdominal infection, pneumonia, cellulitis, and sepsis – prompted its replacement with intravenous amoxicillin/clavulanate (IVAC).
Two studies – one from 1996 and one from 1999 – showed that reducing the use of broad spectrum antibiotics such as PT was associated with reduced incidence of vancomycin-resistant enterococcus (VRE or ‘golden staph’) in hospitals.
New research set out to measure the impact of the PT shortage on VRE and methicillin-resistant Staphylococcus aureus (MRSA) acquisitions at the John Hunter Hospital, where there has been a sustained outbreak of VRE since 2014.
They compared the incidence of hospital-onset acquisitions (hospital-wide) in the 12 months before (October 2016 – September 2017) and 12 months after (November 2017 – October 2018) the start of the PT shortage.
“We found that reducing broad spectrum antibiotic use was associated with reduced VRE transmission and infection,” the team concluded.
“PT has now been reintroduced on a restricted basis and usage remains at a much lower level than before the shortage. We will continue to observe trends in incidence and will also undertake a case–control study of VRE acquisitions.
“Reducing broad spectrum antibiotic use should be a primary goal for hospital antimicrobial stewardship programs.”







 Print
Print